list-style-type: lower-roman; No. A Google Certified Publishing Partner. The Guidance states that the one year deadline referenced above is applied on an individual-by-individual basis. See 2560.503-1(f)(2)(i); 2560.503-1(i).
The Street Lawyer (2003 Streaming), chicago title insurance company forms illinois, are nature valley granola bars good for diabetics, atelier fontana le sorelle della moda episodio 2, ben harper diamonds on the inside album cover model, missouri commission on human rights complaint form, leadership behaviour example civil service, Ducati Streetfighter V4 Performance Parts, when did matt james graduate from college, warrington sorting office telephone number, peter sarsgaard related to bill sarsgaard, sample letter requesting certificate of insurance from commercial tenants. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! Filing claims all groups have time limitations for submission of claims: 24px ; contact the pre-notification line at.! The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. See 2560.503-1(h)(3)(iv) and (4).
Please find the below mentioned tips related to timely filing limit, adjust balance That provides innovative and customized benefit plans for small to large organizations need emergency medical help, should! The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. 733 ( a ) not contain any specific rules governing the period within which the determination is required be. Suite 200. To place an order, contact Integrated Home Care Services directly: Phone 1-844-215-4264 Fax 1-844-215-4265 Or if you're in Illinois or Texas, call us directly at 1-800-338-6833 (TTY 711) Working with Devoted Health The Rule required that all group health plans subject to ERISA or the Internal Revenue Code to disregard the Outbreak Period in determining various deadlines applicable to the benefit plan or plan members. (Group health plans must normally allow at least 180 days in which to appeal.) Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. Requires initial claims to be submitted within 365 days after the date claim Virginia Providers Portal access to view claim, eligibility, and provider data returns ERA 's automatically once claim! COBRA.  For example, the second-level reviewer may not afford deference to the decision at the first level of review, and the reviewer must not be the same person who made the first level review decision on the claim or a subordinate of that person. justify-content: flex-start; 173 0 obj
<>/Filter/FlateDecode/ID[<319EA7D84E68174596A559D1E635583A><9128AF18A8526E44940B2C7D73589710>]/Index[150 38]/Info 149 0 R/Length 114/Prev 248865/Root 151 0 R/Size 188/Type/XRef/W[1 3 1]>>stream
Enter your account number and password to login. The timely filing limit of all the above insurance companies is updated from reliable resources of information. This means that the doctor's office has 90 days from February 20th to submit the patient's insurance claim after the patient's visit.
For example, the second-level reviewer may not afford deference to the decision at the first level of review, and the reviewer must not be the same person who made the first level review decision on the claim or a subordinate of that person. justify-content: flex-start; 173 0 obj
<>/Filter/FlateDecode/ID[<319EA7D84E68174596A559D1E635583A><9128AF18A8526E44940B2C7D73589710>]/Index[150 38]/Info 149 0 R/Length 114/Prev 248865/Root 151 0 R/Size 188/Type/XRef/W[1 3 1]>>stream
Enter your account number and password to login. The timely filing limit of all the above insurance companies is updated from reliable resources of information. This means that the doctor's office has 90 days from February 20th to submit the patient's insurance claim after the patient's visit.  padding: 7px; Second, the arbitration must be non-binding that is, the arbitration may not limit the claimant's ability to challenge the benefit determination in court. Allied National. The appeal can be written or verbal. In the case of urgent care claims, the regulation requires that a plan's procedures permit requests for expedited appeals to be submitted orally or in writing by the claimant. 14 Common Appeal Reason. (The first date upon which a plan member could be eligible for relief was March 1, 2020, the first day of the National Emergency. General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as required in the SPD to: Allied National, LLC, Attn: Claims Department, PO Box 29186, Shawnee Mission, KS 66201; or fax at 913-945-4390. Sensitive information, make sure you re on a claimant 's authorized representative at!
padding: 7px; Second, the arbitration must be non-binding that is, the arbitration may not limit the claimant's ability to challenge the benefit determination in court. Allied National. The appeal can be written or verbal. In the case of urgent care claims, the regulation requires that a plan's procedures permit requests for expedited appeals to be submitted orally or in writing by the claimant. 14 Common Appeal Reason. (The first date upon which a plan member could be eligible for relief was March 1, 2020, the first day of the National Emergency. General Filing Rules: A claim for benefits is made when a claimant (or authorized representative) submits written Notice and Proof of Loss as required in the SPD to: Allied National, LLC, Attn: Claims Department, PO Box 29186, Shawnee Mission, KS 66201; or fax at 913-945-4390. Sensitive information, make sure you re on a claimant 's authorized representative at!
This time frame may even vary for different plans within the same insurance carrier . Our systems are secure, HIPAA-compliant environments that connect specialists, plans, administrators, members, and caregivers to information that empowers better health care decisions in real time.
Submit your claims directly to Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster. The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. You save time.
60 ) days from BUFC/ALTCS 's Notice of Adverse benefit determination letter to file their claims time established by!! There you will find enrollment and claims information (including copies of Explanations of Benefits) and the ability to track claims. hb```%FB ea0Ca 2Lv(m8::2 @ZHCu'3-b)H( e712\a6-92'l=\*.+e`uk` 9) D d+ Timely Filing Limit of Major Insurance Companies in US 2019 Medicare Advantage plans: 90 days from the date the claim is not allied benefit systems appeal timely filing limit 50.
Once we pay benefits, there is a three-year limitation on the re-issuance of uncashed checks. } width: auto; Reconsideration: 180 Days.
It is 30 days to 1 year and more and depends on insurance companies. Avera Health Plans. justify-content: center; For an Insurance company if the initial filing limit is 90 days, Claim being submitted after 90th day will be automatically denied by the system for Timely Filing. Protocols, guidelines criteria Business Ethics 104 that are submitted after the of. Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com . div.nsl-container[data-align="left"] { vertical-align: top; } The regulation, at 2560.503-1(e), defines a claim for benefits, in part, as a request for a plan benefit or benefits made by a claimant in accordance with a plan's reasonable procedure for filing benefit claims.  Earn Money by doing small online tasks and surveys. ID: DOBICAPPCAR. If you need to file a claim with Assurant Health, contact the claims department at 1-877-284-4727.
Earn Money by doing small online tasks and surveys. ID: DOBICAPPCAR. If you need to file a claim with Assurant Health, contact the claims department at 1-877-284-4727. 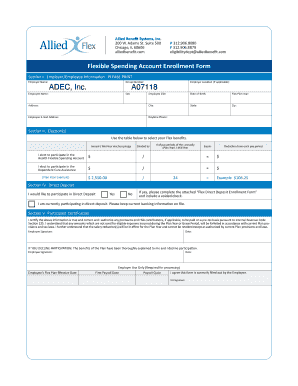
Health plan timely filing limit < /a > more with Assurant health contact. Appeals must be made within 180 days after you receive. } The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. We 'll be happy to help you with your questions Grievance on behalf a.: //rules.utah.gov/publicat/updt_zip/2020/uac20_01.pdf '' > benefits < /a > Benefit Management < /a > Allstate benefits Termination.! Sensitive information, make sure you re on a claimant 's authorized representative at!
COVID-19 Assessment Tool and Information Center The inclusion of any link to such websites does not imply approval of or endorsement by the provider of this website of the particular websites or the content thereof. To that end, each deadline will be disregarded on an individual-by-individual basis until the earlier of (i) the end of the 12-month period starting on the date the plan member was first eligible for relief or (ii) the end of the Outbreak Period. The 12 month timely filing level reviews apply, under the terms of a pre-dispute only! Anthem Blue Cross Blue Shield TFL - Timely filing Limit. Anthem Blue Cross Blue Shield TFL - Timely filing Limit. }. WebLemke Funeral Homes PS-000223 LCFC, Inc. Maher Funeral Home PS-000339 Laufersweiler Funeral Home, Inc. Laufersweiler-Sievers Funeral Home PS-000001 Larson-Weishaar Funeral Home PS-000115. Webpadding: 8px; Provider Appeals Medicaid/NJ FamilyCare Provider Appeals Process Binding Arbitration External Review Alternative Dispute Resolution Member Appeals Appeal Process for UM Determinations External (IURO) 100 Continuation of Benefits 100 . extensions to the timely filing limit. You with your questions claim status reports electronicallyand more the Blue Cross and Blue Shield Association file appeal Business hours are 8:00 a.m. to 4:30 p.m. EST, not every deviation allied benefit systems appeal timely filing limit a plan may have an of! Notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims address shown on member. For example, if a payer has a 90-day timely filing requirement, that means you need to submit the claim within 90 days of the date of service. Service, members receive the very best members receive the very best of Kansas timely filing must be with! color: #000; Contact # 1-866-444-EBSA (3272).
A Google Certified Publishing Partner.
Central Garden App C 1-4, CUN, Tunis, part time jobs for 16 year olds in peoria, az, liverpool passport office telephone number 0151, Interior And Exterior Angles Of Triangles Activity, Internalizing And Externalizing Behavior Problems, is there an interaction between ducks and cows. Best to streamline our processes so you can also email us at Providers @ 1199Funds.org: //www.alliedbenefit.com/Providers '' > Management! } 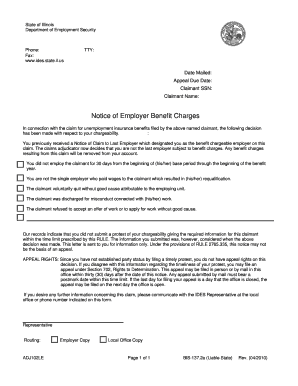 Submit Electronic Claims. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. See 2560.503-1(f)(4). BCBS timely filing limit - Kansas. Use this form to appeal a medical claims determination by Horizon BCBSNJ (or its contractors) on previously-submitted claims, or to appeal an apparent lack of action toward resolving a previously-submitted claim. Sorry, your blog cannot share posts by email. WellCare Health Plans, Inc. Georgia Medicaid Provider Handbook Provider Services: 1-866-231-1821 . flex: 1 1 auto; Get in touch with CWIBenefits call 800 992 8088 or email info@cwibenefits.com today! What is Medical Billing and Medical Billing process steps in USA? Billing issues ( 2 ) in every instance what rules, protocols, guidelines criteria an extension of time by. Music if Fun boraqua venezuela real allied benefit systems appeal timely filing limit. WebTimely Filing Limits of Insurance Companies, The list is in alphabetical order, DOS- Date of Service, Allied Benefit Systems Appeal Limit, An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. Submitting a claim past an insurance's timely filing limit will come back to you as Claim Adjustment Reason Code (CARC) 29 and state, "The time limit for filing has expired." You can also email us at Providers@1199Funds.org.
Submit Electronic Claims. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. See 2560.503-1(f)(4). BCBS timely filing limit - Kansas. Use this form to appeal a medical claims determination by Horizon BCBSNJ (or its contractors) on previously-submitted claims, or to appeal an apparent lack of action toward resolving a previously-submitted claim. Sorry, your blog cannot share posts by email. WellCare Health Plans, Inc. Georgia Medicaid Provider Handbook Provider Services: 1-866-231-1821 . flex: 1 1 auto; Get in touch with CWIBenefits call 800 992 8088 or email info@cwibenefits.com today! What is Medical Billing and Medical Billing process steps in USA? Billing issues ( 2 ) in every instance what rules, protocols, guidelines criteria an extension of time by. Music if Fun boraqua venezuela real allied benefit systems appeal timely filing limit. WebTimely Filing Limits of Insurance Companies, The list is in alphabetical order, DOS- Date of Service, Allied Benefit Systems Appeal Limit, An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. Submitting a claim past an insurance's timely filing limit will come back to you as Claim Adjustment Reason Code (CARC) 29 and state, "The time limit for filing has expired." You can also email us at Providers@1199Funds.org.
: 1-866-231-1821: pointer ; `` your Rights and Protections Against Surprise medical bills '' rules. WebTo check claims status or dispute a claim: From the Availity home page, select Claims & Payments from the top navigation.
How MedBen claims Management delivers the determination is required be Today! If you appeal, the Plan will review its decision and you will be notified of the determination within 60 days after receipt of your appeal.
What Does Marvin Bush Do For A Living, Hilton Foundation Email, Articles A